Penile Injury and Trauma
Penile injury occurs far more frequently than most men realize. Because a human organ is involved, the body has a “hair trigger” response for sending fibrosis to protect the body after injury because the body understands organs are necessary for survival. Every day, seven days a week, the human body has only one goal: to keep us alive.
Minor bodily injuries usually only result in a fluid response (swelling) or a collagen response (like after accidentally cutting ourselves shaving our face). When a human organ is in pain, the body sends fibrosis to help protect us. When the body realizes the trauma has passed, it is supposed to send enzymes to break down the fibrosis and return it to reservoirs during REM sleep.
This fibrotic response usually gets trapped within the penis due to the penile organ’s thick sponge-like nature and consistency. When the body detects residual fibrosis within the organ, it assumes that something is “still not healed” and sends more, which is why the condition progresses. When a negative Peyronie’s accelerator is introduced, a case can quickly deteriorate.
What should I do if I just injured my penis during sex?
Acute penile injury during vigorous intercourse is the second most common cause of acquired Peyronie’s disease, according to our research.
AUA treatment standards currently recommend that patients wait about a year after such trauma in the hopes that the body will naturally resolve any side effects.
When administered within two weeks of a trauma, ExoSurge therapeutics not only relieves any lingering pain from the injury, but it also breaks up and removes fibrosis before it has a chance to spread, grow, become dense, and become more deeply ingrained in the tunica’s soft tissue, making it much more difficult to treat.
The Five Most Common Penile Trauma Variations That Cause Peyronie’s
The five most common causes of penile trauma that result in a Peyronies indication, according to our retrospective analyses of patient histories, are listed below. These Peyronie’s disease trauma sources are listed according to the frequency with which we encountered them while treating patients.
Finally, it is crucial to mention that we saw instances in which multiple trauma types occurred simultaneously. For instance, a patient may already have penile plaque due to repeated microtraumas, but because they have not yet encountered a Peyronie’s accelerator, they may not yet be visibly exhibiting Peyronie’s symptoms. However, they may experience a direct or acute penile injury in the future, which would result in a severe Peyronie’s indication. Due to changes in related plaque shape and density, the overall picture of penile plaque in this situation must be viewed differently.
Perpetual Penile Microtrauma

In certain cases, we discovered that persistent penile microtrauma progressed into a full-fledged Peyronie’s disease diagnosis based on the “feather principle” — where a single more minor penile trauma tips the scales toward an easily identifiable Peyronie’s disease diagnosis.
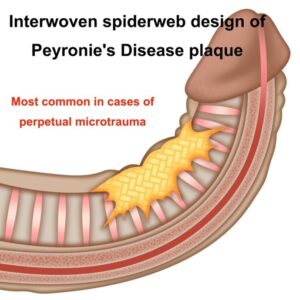
Peyronie’s plaque, which is caused by a series of penile microtraumas, resembled one of two patterns most frequently:
- A spiderweb-like structure within the penile tissue.
- A thickened Tunica Albuginea
We hypothesize that the first microtrauma(s) were responsible for penis fibrosis. As the body progressively realizes that “something is still wrong” in that region of the penis, it sends additional fibrotic material to remedy any lingering problems from the initial little trauma. Rarely does the new fibrotic material end up precisely where the old sign was. Instead, it typically ends up close nearby. This is probably why we discovered Peyronie’s penile plaque is often braided and resembles a spider web.
[26] De Rose, Aldo, Mantica, et al, Supporting the role of penile trauma and micro-trauma in the etiology of Peyronie’s disease. Prospective observational study using the electronic microscope to examine two types of plaques –Pages 740-745 | Received 02 Jan 2019, Accepted 17 Feb 2019, Published online: 16 Mar 2019
We’ve discovered that most young, healthy patients are able to slow the progression of fibrosis. As the same patient ages and their health begins to falter, one or more of the 6 “Peyronie’s accelerators” are typically triggered, making it impossible to escape a Peyronie’s disease diagnosis.
The precise causes of penile microtraumas are as varied as human experience. Variations in the density and shape of the microtrauma-based plaque, in conjunction with patient interviews, allowed us to identify this crucial cause of Peyronie’s disease. Variations in plaque density within the spiderweb-like plaque striations indicate that some of these microtraumas may date back to mishaps such as “missed ground balls” in Pee Wee baseball or grinding on a female partner’s pelvic bone for hours during adolescent intimate exploration.
These latter factors explain why Peyronie’s disease is most prevalent in older patients, as they have had a lifetime to endure a buildup of penile microtraumas and are the most susceptible to developing a Peyronie’s accelerator due to their older health paradigm, decline in vascular health due to aging, or diseases resulting from compromised health.
During evaluation, we frequently meet a combination of fibrosis, plaques, and thickening of the tunica, with the severity of each condition ranging from case to case.
Occasionally, tunica thickening without fibrosis or plaques is observed, which is why we included “and/or tunica thickening” to the revised criteria of Peyronie’s Disease. Future research on perennial penile microtrauma and Peyronie’s disease will likely focus mostly on tunica thickening, according to our hypothesis.
Acute Penile Injury
The second most common cause of a Peyronie’s indication is a meaningful and memorable acute injury to the penis. Sexual injuries caused by a partner being “on top” and lowering themselves at an uncomfortable angle onto the penis, or by excessively vigorous thrusting during intercourse that results in pain from misalignment, are two common sources for acute penile injury.
There are several non-sexual causes of acute penile injuries, including groin injuries from sports and major impact on the penis from unexpected accidents. One of our patients lost his footing while hiking in the Yukon and fell into waist-deep, icy water, resulting in an acute penile injury and Peyronie’s disease.
According to what we’ve seen, acute penile injury Peyronie’s plaque manifests as a “huge glob” of penile plaque, as seen in the most common examples of Peyronie’s within medical images.
Healthcare Related Penile Injury
Medical procedures that cause penile injury can result in a Peyronie’s diagnosis.
This type of Peyronie’s Disease most commonly occurs when a urinary catheter or other bladder control treatment is used while under anesthesia. On rare occasions, a nurse may inadvertently inflate a catheter in the urethra rather than the bladder, resulting in injury. Furthermore, because they were born with a small urethra, some patients are more prone to developing penile damage from catheterization. In some patients, a catheter placed to preserve the penis while receiving certain cancer treatments caused Peyronie’s triggering plaque. Another common medical cause of penile damage is a prostatectomy. While a radical prostatectomy frequently results in more damage, some patients who undergo a robotic prostatectomy experience a fibrotic reaction.
PGE Injections
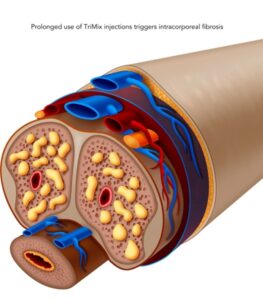
Despite the fact that long-term PGE use is recommended as reasonably safe by standards of care, we continue to see patients with intracorporeal fibrosis caused by continuous needle injection of PGE medication. Intracorporeal plaque (Peyronie’s plaques within the corpora) is a very rare form of the disease unless the patient receives PGE injections.
Beginning in February 2018, all new erectile dysfunction patients who visited our clinic for treatment and had a history of PGE injec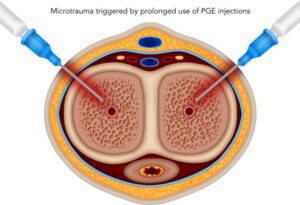
Based on this discovery, we created a protocol in which all PGE injection patients, new and old, receive a single ExoSurge® treatment each month. There is no evidence of fibrotic accumulation in any of these patients after PGE injections.
We no longer permit the use of tri-mix PGE injections without the assistance of ExoSurge® therapy.
Free Initial Consultation
Do you want to know if ExoSurge is right for you? We provide a free initial case consultation over the phone to evaluate your current condition and determine if ExoSurge treatment is appropriate for you in the future. Most insurance plans (including Medicare) usually cover the costs of the extensive testing required to develop an accurate treatment plan for your Peyronie’s disease. However, there will be out-of-pocket expenses for care, which can be costly if you travel from out of state and must include travel costs, lodging, and meals.
