What is Peyronie’s Disease
Lots of patients, doctors and even a drug company who’s constantly hawking their ridiculously high-priced drug on television, define Peyronie’s by a curvature. However, any curvature that appears during erection is just a symptom of the underlying disease, which is the buildup of plaques and fibrosis in the soft tissue of the penis.
Depending upon the exist size and location of the Peyronie’s fibrosis, a penis can curve left, right, up, or down or have little or no curvature at all (35% of our treated patients fell into this category.)
So if Peyronie’s is not a curve, what exactly is it? Based on what we’ve learned so far, we believe the following is the most accurate definition of Peyronie’s Disease.
Peyronie’s Disease Redefined
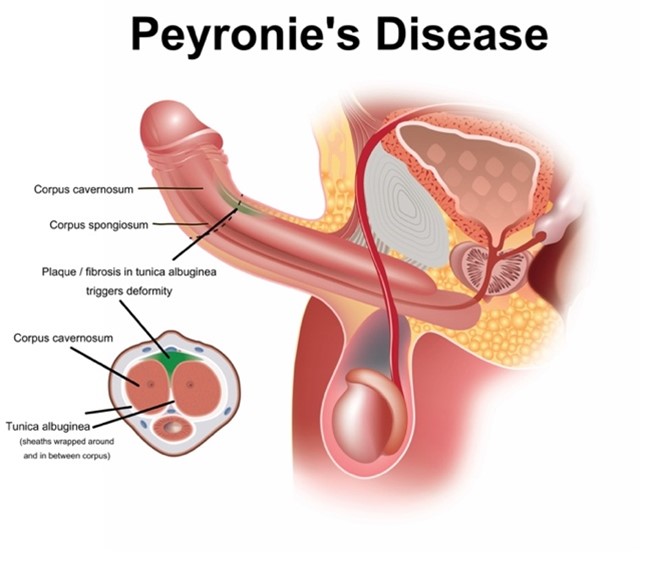
What is Peyronie’s Disease? Peyronie’s Disease (PD) is an acquired inflammatory condition that causes fibrosis in the soft tissue of the penis and/or thickening of the tunica albuginea. In some cases, it is caused by a wound healing disorder.
Let’s dissect this definition because each word is well-thought-out and significant in comparison to other Peyronie’s definitions.
- PD is a “acquired” condition. It is not a hereditary wound healing disorder in 98% of cases. No man is born with Peyronie’s.
- Fibrosis in the penis soft tissue. Ultrasonic technology can see and measure the buildup of fibrosis, plaques, and scar tissue within the soft tissue of the penis. Their exact size and location are what determines all the symptoms Peyronie’s is infamous for.
- A thickened tunica is almost never included in traditional Peyronie’s definitions, but we found its prevalence to be nearly 35% among treated cases, and it causes the same negative side effects as fibrosis.
- Although almost every definition of Peyronie’s disease refers to it as a “wound healing disorder,” we found only a few cases where that was the cause of the diagnosis.
Peyronie’s is not defined by curvature
Contrary to popular belief, we discovered that approximately 35% of treated Peyronie’s patients had little or no curve at the start but always had a clear-cut Peyronie’s diagnosis due to significant and measurable fibrosis and/or plaque in the penis.
Erect curvature is the most common symptom since the easiest pace for fibrosis to form is along the tunica albuginea (the thick sheath that separates the erect organ tissue). As plaque builds up on either side of the tunica, it creates pressure on the opposite side of the penis once the organ is packed full of blood.
Peyronie’s Disease Symptoms
The most common symptoms of Peyronie’s include curvature during erection, nodules4 you can feel with your fingertips just beneath the skin, misshaping of the penis, decrease in penile size, and rings or bands of differentiated tissue around or along the penile shaft. Erectile dysfunction can also occur when the plaque becomes more dense and blocks the natural flow and force of blood required for a full erection.
[4] Chung E, De Young L, Brock GB. Penile duplex ultrasonography in men with Peyronie’s disease: is it veno-occlusive dysfunction or poor cavernosal arterial inflow that contributes to erectile dysfunction? J Sex Med. 2011;8(12):3446–3451
History of Peyronie’s Disease
French surgeon Francois De la Peyronie, Louis XV’s personal physician, made the first clinical diagnosis of Peyronie’s in 1743, but medical publications had been constantly mentioning the ailment since the 1400s. De la Peyronie, who had also personally experienced the syndrome, proposed that it was caused by chronic irritation caused by sexual abuse as well as sexually transmitted diseases.
Peyronie’s is the First Cousin of a Benign Tumor
Peyronie’s plaque is a benign tumor’s first cousin, sharing similarities in appearance, organic growth, and impact on the human body. Peyronie’s fibrotic or plaque material, like the benign tumor, is a non-cancerous mass and can be visually identified and measured from ultrasonography imagery in terms of existing dimensions, growth over time, and/or reduction in size from treatment.
Its removal or reduction is essence to any curative of Peyronie’s Disease outcome. Cutting into it and subsequently manually straightening the penis leaves the fibrosis, meaning the disease and its symptoms can return. Softening it to a point where the penis can be manually straightened leaves the plaques in place, making recurrence a very real possibility in the future. Manually straightening the penis through traction does nothing to remove fibrosis. As the place grows or changes position along the tunica, a curve will and does return.
Can you imagine discovering a tumorous mass in your lung and not monitoring its progress after treatment?
To date, that is the playing field for Peyronie’s care.
How is Peyronie’s Disease Traditionally Treated?
Here we’ll discuss the many traditional methods for treating Peyronie’s disease (including ones we believe to be a complete waste of your time and money).
Oral Medications
No oral medication5 has ever been able to provide measurable reduction in penile fibrosis through independent study, but some patients report improved performance following such regimens.
The medications sometimes employed under standards of care include (alphabetically) Colchicine6, Ibuprofen, L-arginine7, Pentoxifylline, Potassium amino-benzoate and Tadalafil8 and Vitamin E9.
[5] Oral therapy for Peyronie’s: does it work? Brittani Barret-Harlow, Run Wang, Vol. 5, No. 3, June 1, 2016, Translational Andrology and Urology
[6] Safarinejad MR. Therapeutic effects of colchicine in the management of Peyronie’s disease: a randomized double-blind, placebo-controlled study. Int J Impot Res. 2004;16:238
[7] Valente EG, Vernet D, Ferrini MG, et al. L-arginine and phosphodiesterase (PDE) inhibitors counteract fibrosis in the Peyronie’s fibrotic plaque and related fibroblast cultures. Nitric Oxide 2003;9:229-44.
[8] Kovanecz I, Rambhatla A, Ferrini MG, Vernet D, Sanchez S, Rajfer J, et al. Chronic daily tadalafil prevents the corporal fibrosis and veno-occlusive dysfunction that occurs after cavernosal nerve resection. BJU Int 2008;101:203-10.
[9] Safarinejad, M. R., Hosseini, S. Y., Kolahi, A. A. (2007). Comparison of vitamin E and propionyl-l-carnitine, separately or in combination, in patients with early chronic Peyronie’s disease: A double-blind, placebo controlled, randomized study. Journal of Urology, 178, 1398-1403.
List of Medications Taken Orally10
The most common first step many doctors recommend is with oral medications. As evidenced from placebo comparative studies, none have been proven to have any measurable positive effect on Peyronie’s Disease.
[10] Oral therapy for Peyronie’s: does it work? Brittani Barret-Harlow, Run Wang, Vol. 5, No. 3, June 1, 2016, Translational Andrology and Urology
Vitamin E
Because of its mild side effects and low cost, oral vitamin E is a popular treatment for acute stage Peyronie’s disease. While studies dating back to 1948 have shown that vitamin E treatment reduces penile curvature and plaque size, the majority of these studies did not use placebo controls. The few vitamin E studies that included a placebo treatment group revealed that vitamin E did not appear to produce better results than the placebo, raising the question of whether vitamin E is an effective treatment.
Carnitine
An antioxidant medication used to reduce inflammation and thus abnormal wound healing. Uncontrolled trials, like many other Peyronie’s therapies, have shown some benefit to this treatment, but a recent controlled trial has not shown it to be superior to placebo.
Injections into the penile region
Tamoxifen
This non-steroidal anti-estrogen medication has been used to treat desmoid tumors, which are similar to Peyronie’s disease. Unfortunately, placebo-controlled trials of this drug are uncommon, and the few that
have been conducted have failed to demonstrate that Tamoxifen is superior to placebo.
Potassium Amino-Benzoate
Another name for Potaba. Small placebo-controlled studies have shown that this B-complex substance popular in Central Europe improves plaque size but not curvature. Unfortunately, it is somewhat costly, and the medication must be taken 24 hours a day for three to six months. This medication has also been linked to an increased risk of stomach upset. As a result, many men stop taking it.
Colchicine
Colchicine is an anti-inflammatory agent that inhibits collagen formation. In a few small, uncontrolled studies, colchicine was found to be slightly beneficial. Many patients who take colchicine for an extended period of time experience gastrointestinal problems and must discontinue the medication. There is no evidence that Colchicine is superior to placebo.
Intralesional Injections
There are several forms of intralesional injections. Remember the tumor analogy.
Injecting a drug directly into the Peyronie’s disease plaque is an appealing alternative to oral medications. Injection allows drugs to be introduced directly into the plaque, allowing for higher doses and more local effects. A local anesthetic is usually administered prior to the injection to improve patient comfort.
Are there a surgical procedures to heal Peyronie’s disease?
Yes, Peyronie’s surgery11 are considered the “gold standard” according to AUA “standards of care” for Peyronie’s.
However, none of the surgical versions actually “heal” Peyronie’s disease. They erect treats curvature, if present.
Alas, Peyronie’s surgery12 is usually only indicated on cases where the disease completely inhibits sexual activity since most insurance requires that to be the case before surgical intervention is covered.
There are three pathways for Peyronie’s surgery13. We list them by how common each is employed.
Reduce the length of the penis on the side opposite the curve. AKA: Plication14 or Nesbitt. This procedure is the most popular since it has an excellent record for success. In this approach, tissue is trimmed along the curve and subsequently sewn tight, thereby straightening the penis by shortening the outside of the curve. However, all plication surgical versions, it usually results in significant loss of erect length. Versions that incise the plaque (the plaque is not removed, it’s just cut into in order to manually straighten the penis), often result in erectile dysfunction
Make the side of the penis with the curve longer. AKA: Incision and graft15. In this approach, the Peyronie’s plaque is excised, and a graft is transplanted and sewn within the opened area. This approach is popular for men who’ve lost significant length or where the penis shaft is heavily disfigured with indentions. However, a recent ten year retrospective study16 on long term outcomes with Peyronie’s found this version was the most likely to eventually cause recurrence of the disease.
Install a penile prosthetic implant. This approach is suited for men also suffering from erectile dysfunction. In this surgery17, the penis is straightened over an inflatable prosthesis with a pump located in the scrotum. Men can squeeze the pump and achieve erection suitable for intercourse. The biggest complaint18 with an implant is loss of size and rigidity.
[11] Levine LA, Burnett AL. Standard operating procedures for Peyronie’s disease. J Sex Med. 2013;10:230–244.
[12] Levine LA, Burnett AL. Standard operating procedures for Peyronie’s disease. J Sex Med. 2013;10:230–244.
[13] Egydio PH. Surgical treatment of Peyronie’s disease: choosing the best approach to improve patient satisfaction. Asian J Androl. 2008;10:158–166.
[14] Cordon, Billy H., Peyronie’s Penile Plication, Translational Andrology & Urology, 2017 Aug; 6(4): 639–644.
[15] Akkus E, Ozkara H, Alici B, Demirkesen O, Akaydin A, et al. Incision and venous patch graft in the surgical treatment of penile curvature in Peyronie’s disease. Eur Urol. 2001;40:531–6.
[16] Wimpissinger, et al, 10 Years Place and Vein Grafting for Peyronie’s Disease. Does time matter? The Journal of Sexual Medicine, Volume 13, Issue 1, January 2016, Pages 120–128
[17] Garaffa G, Minervini A, Christopher N, et al. The management of residual curvature after penile prosthesis implantation in men with Peyronie’s disease. BJU Int 2011;108:1152-6.
[18] Bonillo M, Garaffa G, Ralph D. Addressing residual penile deformity in the Peyronie’s disease patient during penile implant surgery. Current Sexual Health Report 2007;4:163-6
What are the side effects and issues associated with Peyronie’s surgery?
As mentioned, the big risk with plication is the loss of erect length. Patents often report their new erect length is about where the curve begins. Many patients complain their surgeon did not adequately warn them about the degree of lost length after the fact. There is presently no way to reverse such outcomes.
With incision and graft / veins, the recurrence or loss of quality erections appears to be the biggest risk19.
According to a recent retrospective study published by Florian Wimpissinger, MD, of the department of urology at Rudolfstiftung Hospital in Vienna, Austria in 201220 regarding the long-term outcomes associated with PD surgery, recurrence of Peyronie’s symptoms is a challenge.
After a mean of 9.3 years, the recurrence of postoperative curvature had increased from 0% after a mean of 38 months (18–73 months) to 23.7%, post-op erectile dysfunction increased from 3.0% to 39.5%, penile shortening from 0.0% to 65.8%, and impairment of penile sensitivity from 3% to 31.4%.
“We saw that results tend to worsen with time,” said Dr. Wimpissinger, who presented the study results at the 2011 European Association of Urology annual congress in Vienna.
[19] Ateş K, Salabaş E, Özmez A, et al. Peyronie’s disease surgery: surgical outcomes of 268 cases. Turk J Urol. 2018;44:10–15. [Crossref], [PubMed], [Google Scholar] [20] Urology Times: March 1, 2012: Outcomes of Peyronie’s surgery worsen over time
Free Initial Consultation
Do you want to know if ExoSurge is right for you? We provide a free initial case consultation over the phone to evaluate your current condition and determine if ExoSurge treatment is appropriate for you in the future. Most insurance plans (including Medicare) usually cover the costs of the extensive testing required to develop an accurate treatment plan for your Peyronie’s disease. However, there will be out-of-pocket expenses for care, which can be costly if you travel from out of state and must include travel costs, lodging, and meals.
