Some people are told that silicone injections can make the penis or scrotum look thicker or create permanent “growth.” This is not true. Silicone oil is not safe, does not stay in place, does not create healthy tissue, and often causes severe complications that need reconstructive surgery.
Even when silicone is marketed under names like “permanent filler,” “collagen activator,” “Silikon 1000,” “collagen layering activation,” or even falsely labeled as PMMA, it is still the same unsafe substance.
At Rejuvall, we treat many men who were misled by these claims and later developed painful lumps, deformities, and long-term inflammation.
Why Silicone Oil Does Not Create Real Growth
Silicone injections do not enlarge the penis in a healthy or controlled way. Silicone oil:
- Does not form new collagen
- Does not integrate into tissue
- Does not provide real girth
- Spreads unpredictably
- Damages nerves and blood vessels
- Triggers chronic inflammation
Any temporary “volume” seen early on comes from swelling — not real or stable growth.
How Silicone Is Marketed Under Misleading Names
Silicone promoters often use terms meant to confuse or reassure patients. You may hear:
- “Pharmaceutical-grade silicone”
- “Permanent dermal filler”
- “Collagen layering filler”
- “Silikon 1000 or similar”
- “Permanent filler method”
- “Minimally invasive permanent filler”
- “Permanent girth enhancement filler”
No matter the name, these products all function the same way: they sit in the tissues as foreign material, spread over time, and lead to long-term complications.
The New Trend — Calling Silicone “PMMA”
A growing number of non-urologic providers now call their silicone injections “PMMA”. This is false and dangerous.
Fake “PMMA” usually means:
- Silicone oil
- An unknown, unregulated material
- A substance mixed in the office
- A non-FDA product purchased online
- Material injected without safety testing
Real PMMA = Bellafill®
Bellafill® is the only FDA-approved PMMA-based filler in the United States. It has a long safety record when used correctly by trained physicians.
If a provider cannot show you the Bellafill® packaging, it is not PMMA.
Common Complications from Silicone Injections
Silicone injections can cause serious short-term and long-term problems:
- Hard lumps (granulomas)
- Irregular or uneven shape
- Inflammation and swelling
- Skin breakdown
- Chronic pain
- Loss of sensation
- Migration of silicone into other areas
- Difficulty achieving or maintaining erection
- Necessity for surgical removal and reconstruction
These complications often worsen over time as silicone spreads.
Scrotal enlargement injections and the onset of scrotal lymphedema
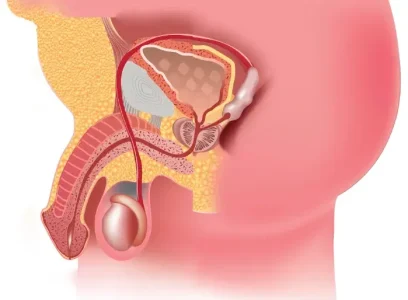
Clinics that thicken a penis by adding bulk to the subcutaneous tissue layers around the penile organ (most commonly with non surgical injections of hyaluronic acid) disrupt the lymphatic drainage system of the penis, but this disruption is easily compensated for by the body’s diversion of lymphatic drainage through the much larger lymphatic drainage system within the scrotum.
However, recently we encountered a patient who’d had injections performed within both his penis shaft and scrotum. According to the patient, he was told by the doctor of the clinic he visited that “these injections caused production of his own collagen”, and that this new collagen would permanently increase the thickness of his penile shaft and size of his scrotum.
This patient’s procedure was performed about six years prior to his recent acute scrotal pain and visit to our urology clinic.
Unfortunately, this patient—like many others—was misled about what was being injected. The provider described the material as a collagen-producing filler, but did not disclose that it was silicone. In some cases, we’ve found clinics use deceptive terminology such as “pharmaceutical grade silicone” to imply safety and medical legitimacy. Let’s be clear: there is no such thing. This is not a regulated medical term. These are unapproved silicone oil injections, and they carry severe health risks.
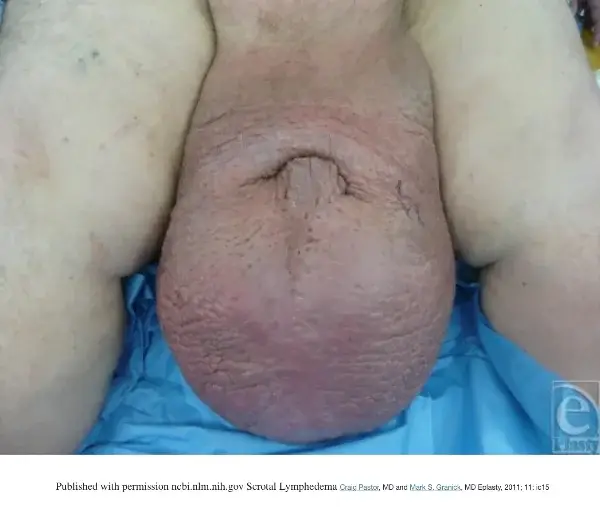
A physical examination revealed that the scrotal region was clearly firmer and more edematous than normal. The damaged areas were all sensitive to touch. A skin biopsy verified the presence of hundreds of microdroplets of silicone in the pelvis as well as the creation of silicone granulomas. Bacterial, fungal, and atypical mycobacterium cultures all yielded negative results.
Injected silicone does not trigger production of life-lasting collagen
Our treated patient was never told that the agent injected to “enhance” his scrotum was silicone. However, even if he had received such informed consent, injected silicone does not trigger collagen production.
The injection of cross-linked hyaluronic acid may be beneficial for stimulating collagen production, according to studies. However, the body’s reaction to injected silicone does not create collagen but rather causes a series of inflammatory responses1 which vary in severity and damage to human tissue.
When liquid silicone is injected into tissue, it forms “microdroplets” of 20 to 100 m2 that are susceptible to gravitational migration. There are two forms of migration, a large-volume silicone that migrates along tissue planes and a small-volume silicone that remains in the tissue and undergoes phagocytosis by macrophages into microdroplets2.
[1] Harlim, Ago et al , Dermatol Surge, 2018 Sep; 44(9): 1174–1182
[2] Lemperle G, Morhenn V, Charrier U. Human histology and persistence of various injectable filler substances for soft tissue augmentation. Aesth Plast Surg 2003;27:354–66.
Smaller silicone microdroplets may endure additional phagocytosis by macrophages and will be transported by lymphatic vessels.
Given that the scrotal lymphatic drainage became blocked by the silicone microdroplets, we observed only large microdroplets in the treated patient, which cannot be phagocytosed and activate macrophages on the silicone surface3. Additionally, the reaction between silicone and tissue produces fibrous chambers and induces granuloma formation.
What is the body’s lymphatic drainage system?
The lymphatic system of the human body is a network of vessels located throughout the body. It returns lymph (fluid), which has leaked from the blood vessels into the tissues, back into the bloodstream through the lymph nodes. The lymphatic system’s role with our health is to regulate the body’s fluid levels.
Lymph nodes are small, kidney-shaped organs that filter body substances. Lymph nodes and lymph tissue contain cells that aid in the fight against infection. There are numerous lymph nodes located throughout your entire body. The most well-known locations for lymph nodes are in the armpits, neck, and pelvis.
The pelvic lymph nodes are located perpendicular to the chest nipples near the hip bone and run angularly above the upper thigh and alongside the groin. From these nodes runs a complex system for fluid drainage, including within the penis shaft and especially within the scrotum. This system filters toxic substances including bacteria, viruses, parasites, and other foreign matter from the body. The lymph fluid can transport cancer cells from these sites to the lymph nodes of the pelvis. Urinary bladder and prostate cancers typically migrate to pelvic lymph nodes.
[3] Rapaport MJ, Vinnik C, Zarem H. Injectable silicone: cause of facial nodules, cellulites, ulceration, and migration. Aesth Plast Surg 1996;20:267.
What is lymphedema?
Definition: Lymphedema is a medical disorder characterized by the accumulation of fluid within subcutaneous fatty tissue.
Lymphedema occurs following an infection or obstruction of the normal drainage of lymphatic channels from the afflicted body part. The affected area of the patient often swell painfully as the growth expands, which can contribute to chronic tissue infection. Most commonly, lymphedema occurs following surgery or radiation treatments for cancer but can also be triggered by conditions such as heart or liver failure.
In the case of our patient, the source of the problem was obstruction of the scrotal lymphatic drainage system through injections of large amounts of silicone oil within the scrotal area. These were most certainly not micro droplet liquid silicone injections in minute quantities of about 0.01 to 0.03mL that some physicians have administered off-label for facial injections. Additionally, the patient was never informed any type of silicone injections were being used, rather it was described as a “collagen inducing injection” that would trigger permanent production of his own collagen.
A man’s scrotal dermis is extremely thin and fragile; it’s akin to the skin of a human eyelid. Injecting this skin with a substance such as silicone causes the dermis to thicken, which would make the patient perceive his scrotum is subsequently “bigger”.
Silicone is a hydrophobic substance that, when injected, disperses in the dermis as droplets, attracting macrophages and large cells that surround the silicone in a foreign body reaction. The emergence of these granulomas can occur months to years after injection and follows an ebbing and flowing cycle of aggravation and remission. The injection of large quantities of silicone exacerbates all of these problems exponentially.
What happens when a patient develops scrotum lymphedema?
Giant Scrotal Lymphedema
In select cases, the scrotum grows to enormous proportions. These cases of significant scrotal growth are characterized as “giant scrotal lymphedema5” and they are devastating.
As a result of the scrotum’s inability to drain the accumulation of fluid from the groin’s lymphatic system, the scrotum’s skin frequently becomes spongy and fluid-laden, thickens, and becomes chronically infected. This makes life extremely difficult for those affected. In the patient we examined for this report, the scrotum had become leathery and dense, and the scrotal drainage system was completely obstructed, backing up residual fluid to the pelvic lymph nodes.
The inability to discharge and filter toxins greatly increases the likelihood of developing testicular or prostate cancer. As a consequence of their condition, patients may become housebound and experience persistent pain.
[4] McDougal SW. Lymphedema of external genitalia. J Urol. 2003;170:711–6.
[5] Vives, Franklin, et, all, Autops Case Rep 2016 Jan-Mar 6(1): 57–61.
Historically, this level of chronic edema of the scrotum has been attributed to conditions such as heart failure, liver failure, lymphatic obstruction, prior surgery, or trauma. For example, patients with kidney failure who receive peritoneal dialysis catheters may develop edema of the scrotum because of drainage from the peritoneal cavity through the inguinal canal and into the scrotum. Surgical evaluation and treatment are the appropriate approaches in such instances.
Silicone injected into the scrotum for “cosmetic enhancement” can lead to serious health complications
Due to reports of potentially catastrophic6 short-, intermediate-, and long-term side effects, liquid injectable silicone (LIS) remains controversial. Silicone is hydrophobic and, when injected, disperses in the dermis as droplets that tend to attract macrophages and giant cells in a foreign body reactio7. The onset of these granulomas can occur anywhere from a few months to many years after injection and follows a distinct pattern of exacerbation and remission.
The extremely fragile and thin scrotal dermis plays a crucial role in supporting lymphatic drainage in the groin. The lymphatic drainage system exists to transport and filter fluids and contaminants that have been excreted throughout the body. This essential drainage system becomes completely obstructed by injections of silicone, which causes scrotal lymphedema.
[6] 2. Christensen L, Breiting V, Janssen M, et al. Adverse reactions to injectable soft tissue permanent fillers. Aesthetic Plast Surg. 2005;29(1):34–48
[7] Altmeyer MD, Anderson LL, Wang AR. Silicone migration and granuloma formation. J Cosmet Dermatol. 2009;8(2):92–97
Insufficiency in the scrotal lymphatic drainage system can result in excruciatingly large growth of the scrotum through the buildup of edema and increases the risk of developing various forms of pelvic cancers.
In this instance, the cause of the problem was lymphatic obstruction in the lower scrotum due to the cosmetic injection of significant quantities of silicone. The patient also stated that “many other men had this procedure,” which would indicate that patients who fail to see a competent urologist immediately following the onset of scrotal lymphedema may develop potentially catastrophic complications in the future.
Treatment: What can be done to repair scrotum lymphedema caused by injected silicone?
Any sort of injected silicone oil is difficult to remove from the human body as the microdroplets can disperse freely within adjacent vascular cells and the bloodstream, which complicates both repair and elimination.
Surgical intervention8 is the best treatment option, offering the possibility of enhanced quality of life for the patient by and restoring urination and possibly sexual function. Once all affected tissue is removed, the scrotum can typically be reconstructed surgically using skin grafts. In most cases, there is sufficient normal tissue surrounding the scrotum to create an acceptable scrotal appearance.
In surgical treatment of prototypical cases of scrotal lymphedema, the penis is submerged in the scrotal tissue and the penis’s foreskin is inverted. Occasionally, penile tissue that has not been affected by lymphedema can be preserved. In some instances, the penile epidermis is also affected and scarred, necessitating its removal. When the penile epidermis must be removed, a skin graft applied to the penis is an option. This will enable the full length of the penis to be exposed, making it less likely that the problem of a buried penis will recur.
Scrotal lymphedema caused by injected silicone creates an especially challenging case. The visible growths from granuloma, the underlying degradation of the fragile scrotal epidermis, and the impossibility of surgically removing all the silicone droplets, makes this new case life threatening for patients who fail to receive appropriate urologic care following the onset of symptoms related to the blocked scrotal lymphatic drainage system and scrotal lymphedema.
[8] Zacharakis E, Dudderidge T, Zacharakis E, Ioannidis E. Surgical repair of idiopathic scrotal elephantiasis. South Med J. 2008;101(2):208–10
Why Rejuvall Uses Only Bellafill®
Rejuvall uses Bellafill®, an FDA-approved PMMA-based filler that helps build natural collagen over time. It does not spread, does not migrate, and has decades of medical safety data.
Bellafill® should never be confused with:
- Silicone oil
- Non-medical PMMA powders
- “Permanent fillers” used by non-urologists
- Anything mixed in a syringe in the office
This difference is critical for safety.
How Rejuvall Treats Silicone Damage
Rejuvall specializes in repairing complications from unsafe injections. Treatment may involve:
- Removing silicone-involved tissue
- Correcting shape deformities
- Restoring sensation and function
- Rebuilding the area using safe, proven techniques
Many of our patients come to us after being told they received “PMMA,” only to later discover it was silicone.
What Safe Options Actually Exist?
The only medically appropriate filler for permanent penile girth enhancement is Bellafill®, used by a board-certified urologic surgeon in a sterile, controlled environment.
Surgery and non-surgical options are individualized based on your anatomy and goals.
Silicone is never a safe substitute.
FAQs
No. Silicone injections are unsafe, unregulated, and often lead to painful lumps, deformity, and chronic inflammation.
Real PMMA = Bellafill®, an FDA-approved filler. Silicone oil is not PMMA and is dangerous when injected.
Some non-urologic injectors mislabel silicone to avoid scrutiny. If it’s not Bellafill®, it’s not real PMMA.
Yes. Rejuvall specializes in repairing silicone damage and restoring normal function and appearance.
Need Help After Silicone or “Permanent Filler” Injections?
If you were injected with silicone, “permanent filler,” or a substance that was described as PMMA, you are not alone — and you are not stuck with the complications.
Many men contact us after discovering that the material they received was not what they were told. Our surgeons specialize in identifying what was injected, treating the inflammation and tissue damage, and restoring both appearance and function with safe, medically proven methods.
Silicone does not dissolve, and it does not become collagen — but the earlier you get expert evaluation, the better your long-term outcome can be.
Speak with our Patient Education Manager for free.
We’ll review your symptoms, your injection history (even if you’re unsure what was used), and discuss the safest next steps.
Fill out the form below to schedule a free phone consultation today and understand your options to protect your health.
If the Cosmetic Urology Assessment form doesn’t appear above, click here to open it in a new window.

Dr. Steven L. Morganstern, M.D.
Dr. Morganstern is an internationally acclaimed, board-certified urologist, surgeon, and best-selling author specializing in men’s sexual health. A pioneer in erectile dysfunction therapeutics, Dr. Morganstern was the only private clinician selected for the original Viagra trials and has spent over four decades advancing treatments in ED, penile enlargement, hormone replacement, and prostate health.




Hello
1. I had a male enhancement procedure done by Dr Loria about 12 years ago. And then I also had another Dr at a different facility a couple years later say that his filler was the same as Dr Loria’s carboxymethylcellulose and ended up putting a HA filler in to try and even out some of the deviations. Needless to say they are extremely different and that’s part of the problem. I hate the different feels of these two fillers. HA wants to float and never becomes my own tissue. I want this HA filler completely removed in certain area’s throughout the penis. Can you remove the HA filler manually? Also the front of the shaft just below the glans is almost 1 inch bigger than the base of the shaft and I want it to be uniformed, so I would need this cut and then stitched back together from approximately midshaft up to the glans roughly, as some of the filler pooled in that area causing it to be larger towards the front of the shaft.
2. It seems like I might fall into not so well of a surgical past like some of your patients. I just watched your videos and it literally repeated the exact same thing that I had previously done. I had the ligament cut but was never told to keep it extended or to put it into a traction device. I also was told that when this doctor cut the ligament that he padded the area where the ligament use to be with adipose tissue. Needless to say I lost about 3/4 of an inch. I was wondering if you could undo what was done? Can you take out that adipose tissue and recut that ligament so I can put it into a traction device or whatever you would recommend? So I would want to do both your surgical and non surgical for length gain.
Please for the love of the almighty help me Dr Carney, I hear great things about your services.
I understand that these 2 procedures might not be able to be done together as the traction device would interfere with the stitches towards the area that’s bigger. I just need help an if two trips are needed so be it.
My direct line is xxx-xxx-xxxx, please message me at your earliest convenience
Hello, Sir and thank you for reaching out. I just spoke with our case consultant, John, and I believe he has actually already reached out to you. If not, please submit the Cosmetic Urology Assessment Form and schedule a call with John. Hopefully we can get you seen very soon. You can find that form at https://www.rejuvall.com/nervous-we-understand/. Thank you again, and we look forward to being able to serve you.
Pingback: Pharmaceutical Grade Silicone Penile Injections – Risks, Myths, and Long-Term Damage
Pingback: What Is a Dominican Dick Lift? Understanding the DDL and Its Risks - Rejuvall